OVERVIEWAs the best bone marrow transplant hospital in India, HCG houses a dedicated hematology and bone marrow transplant department, which comprises experienced and skilled haematologists and BMT specialists who specialise in the diagnosis, treatment, and management of a broad spectrum of benign and malignant disorders of blood and bone marrow.
11
Centers largest network BMT centers
18+
Consultants and 60 nurses - Largest team of trained specialists
1600+
Successful BMTs
All BMT room with separate HEPA filters.
0.3 mm filtered positive airflow with 12 air exchanges per hour.
Largest team based opinion for all complicated and BMT patients.
Benign Hematological Disorders
Red Blood Cell (RBC) Disorders
The key function of red blood cells is to carry oxygen and the disorders that affect these cells are termed red blood cell disorders. Sickle cell anaemia, aplastic anaemia and thalassaemia are common red blood cell disorders.
White Blood Cell (WBC) Disorders
The key function of WBC is to regulate the body’s immune system. WBC disorders are caused by abnormal white blood cells, also known as leukocytes. WBC disorders are characterised by either very high or very low WBC numbers. Neutropenia and MDS are two major white blood cell diseases.
Platelet Disorders
The primary function of platelets is to support wound healing. Platelet disorders are characterised by either very high or very low numbers of platelets. ITP and dengue are two important platelet disorders.
Bleeding Disorders
Bleeding disorders are caused due to multiple factors. When an injury occurs, the blood does not clot, and this can lead to a multitude of health complications. Haemophilia is one of the bleeding disorders.
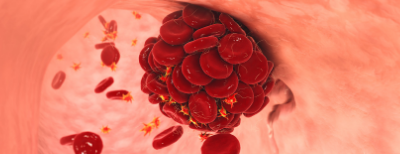
Clotting Disorders
Clotting disorders happen when blood clots unexpectedly in the veins and arteries. This affects the blood flow and functioning of the organs. Deep vein thrombosis refers to the clots forming in legs, and pulmonary embolism refers to the clots forming in the lungs.
Malignant Hematological Disorders/Blood Cancers
Leukaemia happens when bone marrow starts making abnormal white blood cells in excess quantities. These abnormal cells later enter the bloodstream. Important leukaemia types include Acute Myeloid Leukaemia (AML), Acute Lymphocytic Leukaemia (ALL), Chronic Myeloid Leukaemia (CML) And Chronic Lymphocytic Leukaemia (CLL).
Lymphoma starts in infection-fighting cells and is largely seen arising in the lymph nodes, spleen, thymus, and bone marrow. More than 60+ types of lymphoma are identified; nevertheless, it is broadly classified into two types - Hodgkin's Lymphoma & Non-Hodgkin's Lymphoma.
Myeloma is a type of blood malignancy that arises from plasma cells. This cancer largely affects and damages the bones, immune system, kidneys, and red blood cells. Multiple myeloma is the most common type of myeloma.
Early detection and timely treatment play a significant role in the successful management of blood malignancies. It's critical to diagnose and classify the disease correctly with the help of high-end specific tests.
Chemotherapy, radiation therapy and bone marrow transplantation are the common treatment methods used to treat blood cancers.
However, bone marrow transplantation is largely preferred as a curative option when the patient is at a high risk of relapse.
Bone Marrow Transplant
Stem cell transplant or bone marrow transplant is a medical procedure that replaces the destroyed or damaged bone marrow cells or stem cells with healthy bone marrow cells.
It involves the extraction of healthy stem cells, filtration, and transferring them back to the donor itself (auto transplant) or to another individual, who is called the recipient/ donor (allogeneic transplant)

Why is Stem Cell Transplant Required?
The goal of stem cell/ bone marrow transplant is to treat many diseases and a few types of cancer successfully. For some diseases, a stem cell/bone marrow transplant serves as the only potential cure by helping patients have a healthy, functioning marrow.
A stem cell/bone marrow transplant becomes necessary when:
The existing bone marrow cells are damaged, destroyed or not functioning optimally due to health conditions such as aplastic anaemia, leukaemia, etc.
The immune system needs to be regenerated to fight the existing or residual cancers that could not be treated completely with radiation or chemotherapy.
The patient suffers from a health condition that affects the production of bone marrow cells or other serious immune system illnesses.
The normal functioning of the immune system is to be restored after high doses of chemotherapy and radiation that are given to treat malignant health conditions. This transplant, which is known as rescue, replaces the damaged bone marrow with the healthy bone marrow. This is commonly performed in diseases like lymphoma and neuroblastoma.
Types of Bone Marrow Transplant
Bone marrow transplant is categorised depending on the source of the healthy stem cells. In other words, the classification is made based on who the donor is. There are three types of bone marrow transplant:
Autologous Bone Marrow Transplant
As the name says, during an autologous bone marrow transplant, the patient is itself the donor. The stem cells are carefully extracted before the patient receives high-dose radiation or chemotherapy and are stored in the freezer. After the chemotherapy or radiotherapy, the stem cells are put back into the patient’s body, where they start producing normal blood cells.
Allogeneic Bone Marrow Transplant
The term “allo” means different. During an allogeneic bone marrow transplant, the stem cells are extracted from another individual, known as the donor, based on their HLA type (genetic match). The HLA type of the donor’s stem cells should match with the HLA type of the recipient. Allogeneic bone marrow transplant is further classified into two subtypes:
Umbilical Cord Blood Transplant
During an umbilical cord blood transplant, the stem cells are collected from the umbilical cord at the time of the childbirth. These stem cells are tested, typed, and stored until they are used for transplantation.