07 Nov, 2025
Feel free to reach out to us.
07 Nov, 2025

This article is medically reviewed by Dr. Manasi Shah, Consultant - Medical Oncology, HCG Aastha Cancer Centre, Ahmedabad.
20% of the world’s cervical cancer cases are recorded in India, and that’s a lot.
Also, in 2022, India reported the highest number of deaths related to cervical cancer, which stood at 79,906.
Here is something that not many know: Cervical cancer is one of the slow-growing cancers; it takes years to progress from a precancerous condition to cancer. Yet, our country records this cancer in high numbers. Delayed diagnosis is responsible for poor cervical cancer treatment outcomes.
Possible reasons for a high incidence rate could be limited awareness about this cancer and its preventive measures, which is especially true in rural parts of the country.
To address this knowledge gap, we have come up with a comprehensive blog article that discusses what HPV is, how it causes cervical cancer, how the HPV vaccine reduces cervical cancer risk, myths and facts associated with the HPV vaccine, and more.
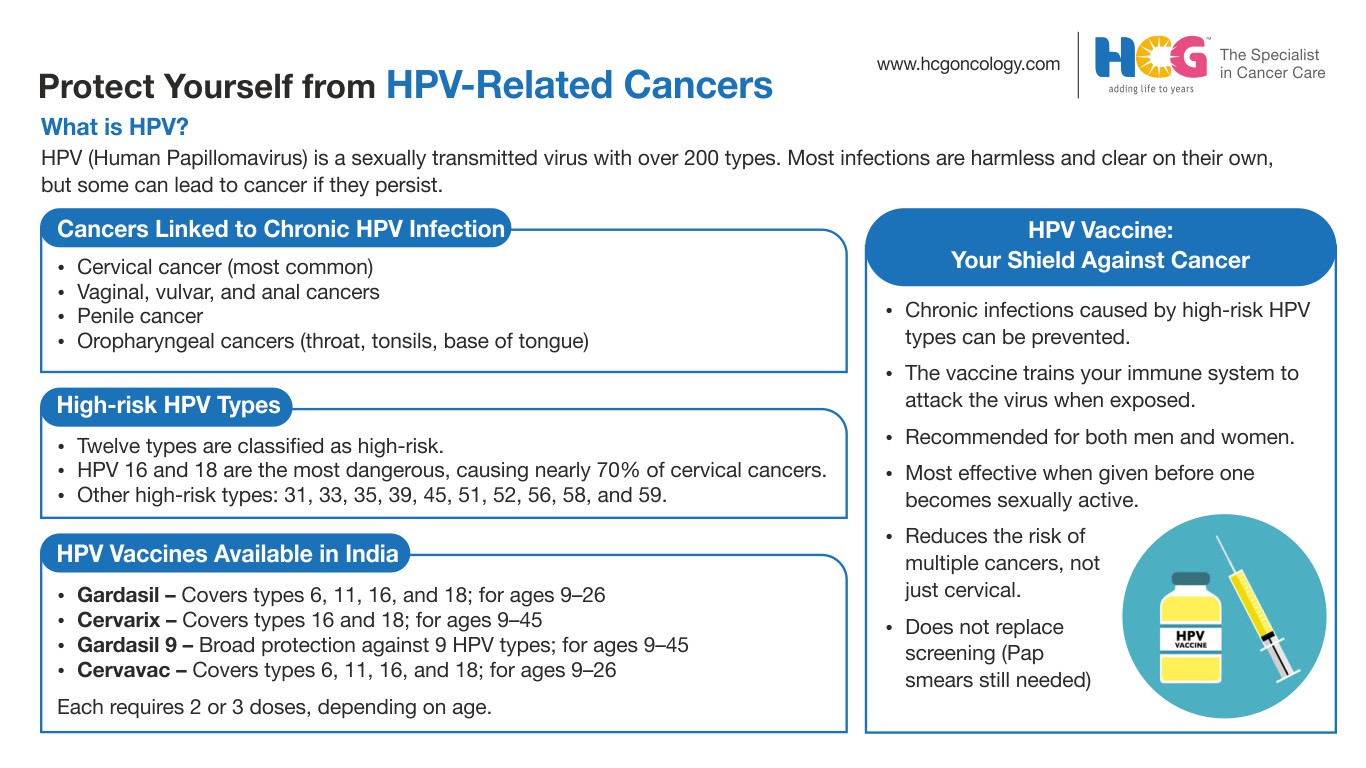
HPV, or human papillomavirus, refers to a group of viruses that are commonly transmitted through sexual contact. About 200 types of HPV have been identified, of which 12 types have been recognized as “high-risk” types with the potential to cause different types of anogenital cancers, and they include HPV 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, and 59.
HPV infections are very common, and nearly all individuals who are sexually active contract them at least once in their lives.
In about 80-90% of cases, this infection is self-limiting, i.e., it clears within 1-2 years by itself, thanks to our immune system. However, in some cases, this infection can become chronic.
When HPV infections become chronic, they alter the way the cervical cells grow and multiply.
Over time, these changes lead to mutations in cervical cells and cause them to divide abnormally, leading to precancerous changes and cervical cancer eventually. It may take anywhere between 5 and 20 years for the precancerous changes to develop into cervical cancer.
Various factors can contribute to the rate at which cervical cancer develops from precancerous changes, and they are referred to as risk factors.
Common risk factors associated with cervical cancer development include a weakened immune system, smoking, early sexual activity, multiple sexual partners, coinfection with other sexually transmitted diseases, prolonged use of contraceptives, obesity, and more.
Cervical cancer is the second most common cancer among Indian women, contributing to 17.7% of the total cancer burden. Studies suggest that about 70-90% of cervical cancer cases are associated with high-risk HPV infections.
That said, not all women with an HPV infection develop cervical cancer.
According to reports, in about 10% of women, HPV infections become chronic and lead to cervical cancer development. In the remaining 90% of women, HPV infections clear on their own with the help of the body’s natural defense.
As mentioned earlier, about 12 types of HPV have been identified with the potential to cause various types of anogenital cancers, namely cervical, vulval, vaginal, anal and oropharyngeal cancers. Of them, HPV types 16 and 18 cause the highest percentage of cervical cancer cases.
The key to reducing the risk of cervical cancer lies in adopting preventive measures against high-risk HPV types.
Additional Reading: 8 Ways To Reduce Your Cervical Cancer Risk
In this section, we answer the burning question, “How to avoid cervical cancer?” or “How to reduce the risk of cervical cancer?”
With a few simple measures, it is possible to reduce cervical cancer risk. And they include Pap smears and HPV vaccinations.
Pap smears, a type of screening test, help reduce the risk of cervical cancer by detecting precancerous lesions caused by HPV infections. However, the development of HPV vaccines has created opportunities for more effective cervical cancer prevention.
The following are the different HPV vaccines available that can help in preventing HPV infections and reducing the risk of cervical cancers:
Success rates of HPV vaccines against all HPV-related cancers, including cervical cancer, stand between 80% and 100%.
Numerous studies have examined the relationship between the HPV vaccine and cervical cancer rates. Here are some intriguing insights gathered from research across the globe that analyzed cervical cancer rates before and after the HPV vaccine.
In this section, we explore the impact of the HPV vaccine on cervical cancer.
Human papillomavirus (HPV) vaccines work just like other immunizations. These vaccines contain purified, inactive protein particles from the virus. These particles can trigger the formation of HPV-specific antibodies or other immune mechanisms.
This way, when the infection actually occurs, your immune system is ready to fight against it. This vaccine effectively curbs persistent HPV infections and thereby helps in preventing the formation of precancerous lesions and subsequent cancer development.
However, HPV vaccination should be considered a preventive measure only and not as a treatment method for precancerous conditions or cancer itself. Additionally, HPV vaccines should not replace cervical cancer screening, as it can be caused by other risk factors, too.
HPV vaccination does not cause any major side effects. However, in rare cases, pain, swelling, itching, bruising, redness at the injection site, headache, fever, nausea, dizziness, vomiting, and fainting could be observed, which wear off after some time.
The human papillomavirus vaccines are surrounded by various myths that can give rise to unwarranted fear and hesitation, deterring people from getting vaccinated.
In this section, let’s bust some common myths and understand crucial facts associated with human papillomavirus vaccines:
Fact: The HPV vaccine is highly effective in reducing the risk of HPV-related cancers, such as cervical cancer. However, it does not offer 100% protection.
Fact: The HPV vaccine does not replace cervical cancer screening. It is still required after taking the vaccination, as it helps in detecting precancerous changes in early stages.
Fact: Both men and women should get the HPV vaccine anytime between the ages of 9 and 45.
Fact: If someone is affected by one strain of HPV, the vaccine can offer protection against other HPV strains.
Fact: The HPV vaccine does not cause infertility. The human papillomavirus vaccines are extensively studied for their safety and efficacy, and no study has reported that they cause infertility or any other debilitating side effects.
Fact: The HPV vaccines are specifically designed to target strains known to cause cervical and other anogenital cancers.
Vaccination helps trigger a targeted immune response against these strains, unlike natural infections, which can result from any of the 200 HPV strains.
Additional Reading: Are you reducing your risk of getting Cervical Cancer? | HCG
Australia was the first country to introduce a national HPV vaccination program to achieve the elimination of cervical cancer. Such programs are necessary for countries like India, where the incidence is high.
Globally, the WHO has set a 90/70/90 target that is to be achieved by 2030. As per this program, 90% of adolescents shall be vaccinated, 70% of women will be screened for HPV at least twice in their lifetime, and 90% of women will be treated effectively for precancerous lesions or cancer itself.
In 2023, India’s first indigenous HPV vaccine, Cervavac, was launched by the Serum Institute of India. This is a gender-neutral vaccine that is effective against the strains of HPV 6, 11, 16, and 18.
In 2024, HPV vaccination received a budget push by the Government of India, where the finance minister spoke about how the government encouraged HPV vaccination for girls between the ages of 9 and 14 and how it intended to include the HPV vaccine in the national vaccination program.
That said, awareness among the masses is the key to beating any disease. Awareness of cervical cancer should be created on both individual and community levels, through which the risk of cervical cancer can be successfully brought down among women.
Both men and women should get the HPV vaccine. Ideally, this vaccine should be taken before getting exposed to human papillomavirus, i.e., before one becomes sexually active. That said, in certain circumstances, taking the HPV vaccine after exposure helps achieve protection against certain high-risk HPV types.
All major human papillomavirus vaccines available in India can be taken between the ages of 9 and 45.
Since a large percentage of cervical cancer cases are caused by chronic HPV infection, the key to the prevention and control of cervical cancer lies in preventing chronic HPV infection.
The HPV vaccine reduces cervical cancer risk, along with the risk of other anogenital cancers, by preventing chronic infections. The HPV vaccine can be taken between the ages of 9 and 45 by both men and women.
There are 4 types of HPV vaccines available in India, and they are all effective against the high-risk types of HPV 16 and 18.
HCG urges all men and women to consider getting vaccinated against HPV to put themselves a step ahead of various types of anogenital cancers and oropharyngeal cancers.

Dr. Manasi Shah
Consultant – Medical Oncology
MBBS, American Board Certified in Internal Medicine, American Board Certified in Medical Oncology and
Hematology
Dr. Manasi Shah is an experienced medical oncology consultant from HCG Aastha Cancer Centre, a leading cancer hospital in Ahmedabad, and she specializes in cancer management through systemic therapies. Her expertise lies in treating breast and gynecological malignancies, including ovarian, uterine, and cervical cancers, using chemotherapy, targeted therapy, immunotherapy, and hormone therapy. She is also a part of several national and international trials, working to improve the standard of care for cancer patients in India and to improve access to newer drugs.
Appointment Link: Book an Appointment with Dr. Manasi Shah.